The incidence of thyroid cancer in the US is growing rapidly — more rapidly than that of any other cancer. Although this might seem like a cause for concern, surprisingly, it’s not. While the incidence is rising, the mortality from thyroid cancer hasn’t increased in over 35 years. And the reason mortality rates have stayed so low — despite the increased number of cases– has nothing to do with improved thyroid cancer treatment: In fact, treatment hasn’t substantially changed in years.
So why are thyroid cancer mortality rates so low?
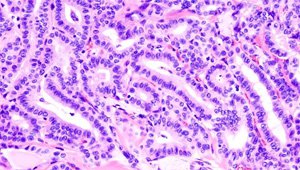
What we have gotten good at is detecting thyroid cancer. While detection doesn’t always translate into a better outcome when you’re dealing with a very serious disease, most thyroid cancers — as many as 85 percent — are papillary cancers, a reference to their distinctive appearance under the microscope. These cancers are very slow-growing when they grow at all, and spread even less often, and thus only rarely impact a patient’s overall health and lifespan.
How is thyroid cancer detected?
Thyroid cancer is most often detected during a physical exam as small nodules on the neck. The vast majority of patients are completely without any symptoms unless the nodule is so large that it is pressing against other structures in the neck, such as the esophagus — making it hard or painful to swallow — or larynx — making it difficult to breathe. The rest of the thyroid gland usually functions normally, so the patient doesn’t have hypothyroidism or hyperthyroidism symptoms.
Once a nodule is detected, patients are sent for an imaging study such as an ultrasound. If the lesion looks suspicious for cancer, it is biopsied. However, it’s important to note that in almost all cases of papillary cancer, detection and treatment with surgery and radioiodine makes no difference in the patient’s overall mortality. For most patients, the major impact of finding these slow-growing cancers means subjecting them to an invasive procedure with potential side effects, in addition to a lifetime of anxiety that a cancer diagnosis brings.
So what do doctors recommend for thyroid cancer treatment?
By treating these papillary cancers, are we really doing our patients any favors? In most cases, the answer is “no.” Over 60,000 new cases of thyroid cancer will be detected this year while the annual mortality from the disease is steady at about 2,000, the same number that it has been for decades. Many clinicians are now advocating that patients with papillary thyroid cancer do not need to be treated aggressively. Instead, they can be followed with serial ultrasounds and only treated if there is worrisome evidence of growth or spread. Patients with more aggressive types of thyroid cancer still need treatment, however.
Simply identifying a lesion as thyroid cancer, even with the knowledge that it is highly unlikely to cause any problems, is a source of great distress to many patients. Not screening for thyroid nodules at all is an option that is being explored, but no one is yet ready to advocate eliminating it altogether. Further research is examining whether this option is tenable.
I have papillary thyroid cancer – Should I be worried?
For now, the bottom line is that the majority of thyroid cancers never become clinically significant. Some experts are even advocating that we no longer even call them cancers at all. Should you or your health care provider find a thyroid nodule that proves to be a papillary cancer, then together you can decide which is the best approach for you—to go ahead and aggressively treat it, or follow it closely with serial ultrasounds.
Don’t miss the rest in our series on thyroid health, beginning with Everything You Need to Know About Your Thyroid.
The One Medical blog is published by One Medical, a national, modern primary care practice pairing 24/7 virtual care services with inviting and convenient in-person care at over 100 locations across the U.S. One Medical is on a mission to transform health care for all through a human-centered, technology-powered approach to caring for people at every stage of life.
Any general advice posted on our blog, website, or app is for informational purposes only and is not intended to replace or substitute for any medical or other advice. 1Life Healthcare, Inc. and the One Medical entities make no representations or warranties and expressly disclaim any and all liability concerning any treatment, action by, or effect on any person following the general information offered or provided within or through the blog, website, or app. If you have specific concerns or a situation arises in which you require medical advice, you should consult with an appropriately trained and qualified medical services provider.